Dispelling myths around
lower back pain
Part One
Adapted from: O'Sullivan, P. B., Caneiro, J. P., O'Sullivan, K., Lin, I., Bunzli, S., Wernli, K., & O'Keeffe, M. (2020). Back to basics: 10 facts every person should know about back pain. British journal of sports medicine, 54(12), 698-699.
Low back pain is one of the most common musculoskeletal (MSK) conditions seen within physiotherapy clinics, with data suggesting over any given one-month period, close to one-third of people aged over 25 are living with low back pain in the UK [1]. Given its prevalence, many theories exist around the causes of low back pain and how best to manage it. It’s an area of significant research, given the impact it can have on an individual, but also the wider social and economic effects of low back pain. Appointments and consultations relating to low back pain cost the NHS almost £5 billion pounds a year [2]. Consequently, there is a significant amount of misinformation relating to low back pain. In this blog, we will look at some commonly reported beliefs in low back pain and how many may not be entirely accurate.
Myth 1 - "Low Back Pain Is A Serious Health Condition"
Acute or persistent low back pain can be extremely distressing and debilitating for the individual living with it. However – it is rarely caused by serious pathology. Data from Australia identifies that between 90-95% of people presenting to their GP were diagnosed with non-specific low back pain (NSLBP) [3]. Whilst NSLBP is actually very specific (to the individual experiencing it), this diagnosis is given where a specific cause of back pain cannot be identified via symptom history, assessment, or scanning. Importantly, this diagnosis excludes serious or sinister pathology that is only present in around 1% of new onset low back pain. NSLBP encompasses pain that may arise from the soft tissues (muscles, ligaments, tendons), discs or joints within the low back. We know symptoms arising from these structures generally have a favourable outcome, with most people finding significant improvement within the first 8-12 weeks of symptoms.
In clinic, sometimes I explain this similarly to catching a common cold. It is something that many people can regularly experience, sometimes for a known cause (for example, our partner has had a cold recently) but more often without a clear reason. The same can be true for a flare of low back pain, that sometimes we can attribute its onset to a specific task or activity but more commonly symptoms appear without clear cause. When we catch a cold, we do not automatically assume it is the beginning of pneumonia. In many cases, with time and the right management, your cold symptoms improve, and this is the same for a majority of flares of low back pain.
Myth 2 – “As I get older, my low back pain will worsen with time”
Whilst people commonly believe we are more susceptible to developing low back pain as we age, there is no convincing large-scale evidence to suggest that this is true. Data from the World Health Organization reports peak prevalence of reported low back pain symptoms is between the ages of 50-55 [4] and that cases reduce past this age. It could be suggested that as we move past these ages and for some towards retirement, that we are more able at this stage of life to manage low back pain more effectively through alterations to lifestyle factors, reduced workplace stress and improved overall quality of life.
Myth 3 – “Persistent low back pain must be linked to tissue damage”
The back is an incredibly strong, stable, and resilient structure. We know from decades of research into healing processes within the body, that tissue healing occurs over roughly a three-month period in a typical individual. We then understand that if pain persists past this point, the reliability of this message must be questioned and that perhaps other factors may contribute to why this pain continues.
There are many examples of common circumstances where the brain produces pain signals, but that this is not equivalent to the level of tissue damage. A paper cut can be extremely painful acutely, but the damage to the tissues conversely is very small. Headaches can be very painful for those experiencing them, but no damage to tissues within the body occurs. An extremely important message in low back pain that has persisted past the healing timescales, is that the pain is absolutely real. But also, that this real pain message is very unlikely equivalent to what is occurring within the tissues of your low back.
When supporting an individual with persistent low back pain, we know that treating the person “as a whole” or what we would call clinically as a biopsychosocial approach, is vitally important. Research specifically into low back pain suggests the strongest predictive factors of chronic back pain are closely linked to psychology. These include anxiety and depression, which can occur where back pain limits our ability to engage in hobbies, activities or maintain meaningful relationships. Increased stress, poorer sleep, and general health factors such as raised body weight, smoking status and reduced baseline levels of general activity are also associated within an increased risk of persistent symptoms [5]. It is therefore important when assessing a person with persistent low back pain, that as clinicians we look at the bigger picture when creating a plan to support you.
Myth 4 – “Having an X-Ray/CT/MRI scan will tell us why I have low back pain”
Scans are very often not required in the diagnosis of low back pain conditions. Scans will commonly reveal what could be perceived to be quite scary changes within the lumbar spine, such as changes to the height or density of spinal discs, changes to the position of the discs (e.g, “bulges”) and conditions such as arthritis within the joints. What the reports of these scans fail to mention, is that these changes are also very commonly seen in people without pain. A study [6] of over 1000 people without back or leg pain found that if we are over the age of 30, it is statistically more likely than not that we will have some findings on an MRI scan (see table below). It is also important to understand that any scan of your spine is relevant to the moment it was taken, and that time only. A vast majority of disc bulges are shown in research to resolve spontaneously without the requirement of any specific treatment [7]. As they become statistically increasingly prevalent with age, these changes can be attributable to the aging process. Other examples of this can be the grey hairs that start appearing (but between us, I was never-the-less disappointed to see these at 29 years old) or skin that has more wrinkles. When this occurs, we do not panic as we expect to see these changes.
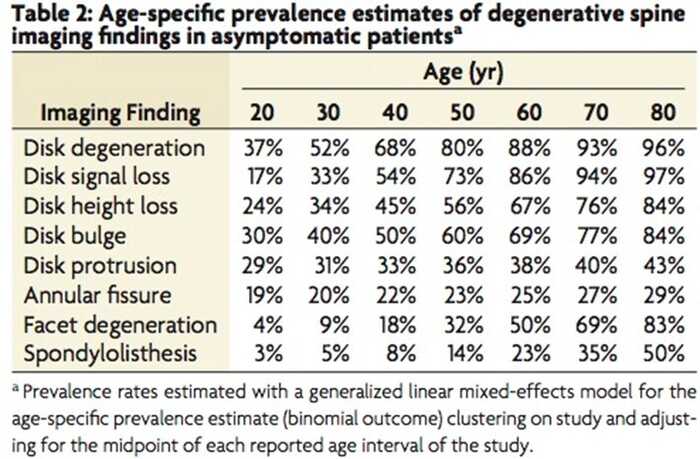
It is of course though also reasonable to assume that some changes that may be classified as “age related”, such as those listed in the table above, can cause flares of low back pain. The science behind why some people feel pain with these changes and others do not, is not fully understood. It is extremely likely that this is multifactorial, in that there are many reasons why rather than one alone. One proposed theory is that if these changes occur gradually, rather than suddenly, the brain’s internal filtering system does not perceive a threat. Consequently, pain messages are not produced but the changes can be seen on imaging. The presence of any of these features do not affect the strength or stability of your spine and it is safe to continue with normal activities.
Myth 5 – “If I keep feeling pain during exercise I must stop as this means I could damage my spine”
Pain is an experience produced by the brain in response to a stimulus that it perceives to be a threat. For example, if you put your hand on a hot stove, you receive pain messages instantly from your brain to move your hand to prevent damage. In this circumstance, pain messages have produced a positive result in that they have protected you from further harm. As we have discussed previously, in persistent pain whilst the pain messages are real, they have lost their protective mechanism. Examples of this can be pain that occurs with simple everyday tasks such as standing or bending, or even when lightly touching the spine. We know these examples are not causing harm to the spine, but real pain is felt.
Pain during activity, movement or exercise actually more closely represents how sensitive the structures in your low back are, rather than how damaged they are. So, it is safe for someone to feel some pain when starting to move and exercise more. Research strongly suggests that gradually increasing activity and exercise improves control of symptoms in low back pain. A physiotherapist can tailor a specific plan to help you return to activities and sport that you value, as well as educating you in understanding how to appropriately work into acceptable symptoms. The benefits of exercise can be increasing tolerance and resilience to spinal movements and positively influencing the strength and endurance of spinal tissues.
Join me in part two where we will discuss five more common myths relating to lumbar back pain.
References
[1] GBD 2021 Low Back Pain Collaborators. (2023). Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. The Lancet. Rheumatology, 5(6), e316.
[2] Macfarlane, G.J., Beasley, M., Jones, E.A., et al. (2012) The prevalence and management of low back pain across adulthood: results from a population-based cross-sectional study (the MUSICIAN study). Pain 153(1), 27-32.
[3] Bardin, L.D., King, P. and Maher, C.G. (2017) Diagnostic triage for low back pain: a practical approach for primary care. Medical Journal of Australia 206(6), 268-273.
[4] webpage: Low back pain (who.int) – World Health Organization – link checked on 22nd May 2024.
[5] O'Keeffe, M., O'Sullivan, P., Purtill, H., Bargary, N., & O'Sullivan, K. (2020). Cognitive functional therapy compared with a group-based exercise and education intervention for chronic low back pain: a multicentre randomised controlled trial (RCT). British journal of sports medicine, 54(13), 782-789.
[6] Brinjikji, W., Luetmer, P. H., Comstock, B., Bresnahan, B. W., Chen, L. E., Deyo, R. A., ... & Jarvik, J. G. (2015). Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. American journal of neuroradiology, 36(4), 811-816.
[7] Yu, Pengfei, Feng Mao, Jingyun Chen, Xiaoying Ma, Yuxiang Dai, Guanhong Liu, Feng Dai, and Jingtao Liu. "Characteristics and mechanisms of resorption in lumbar disc herniation." Arthritis Research & Therapy 24, no. 1 (2022): 205.
Posted by Jack Thomas on May 29th 2024
